Child & Teen BMI Calculator
Enter your child’s height, weight, and age to calculate their BMI and percentile. Plus, see their body mass classification, according to the CDC growth percentile charts.
Child's Body Mass Index (BMI):
On this page:
How to Calculate BMI for Children
BMI, or body mass index, is a helpful tool for determining weight and health status for both adults and children. It is a simple formula that uses height and weight to provide you with an idea of where your child falls within certain weight categories.[1]
To calculate BMI, you only need to know your child’s current height and weight. The formula for BMI is:
BMI = weight [kg] / height² [m²]
Imperial Units
BMI = weight [lb] / height² [in²] × 703
The formula for BMI is the same for adults and children. However, the value is interpreted differently in children. In kids and teenagers, BMI is age and sex-specific.
This is because body fat and weight standards change with age and sex due to different body structure and hormone fluctuations.
As an example, an 8-year-old girl with a BMI of 22 would fall into the greater than 95th percentile and would be considered obese.[2] However, a 15-year-old girl with a BMI of 22 would fall between the 50th and 75th percentile and would be considered to be a healthy weight.[2]
These BMI charts are available on the CDC website (boys[3] and girls[4]).
Body mass index for-age growth charts from the CDC take into account these differences and show BMI as a percentile ranking rather than falling into underweight, normal weight, or obese categories that are used in adults.
These values were based on data collected from surveys of children from the U.S. population from 1963-65 to 1988-94.[1]
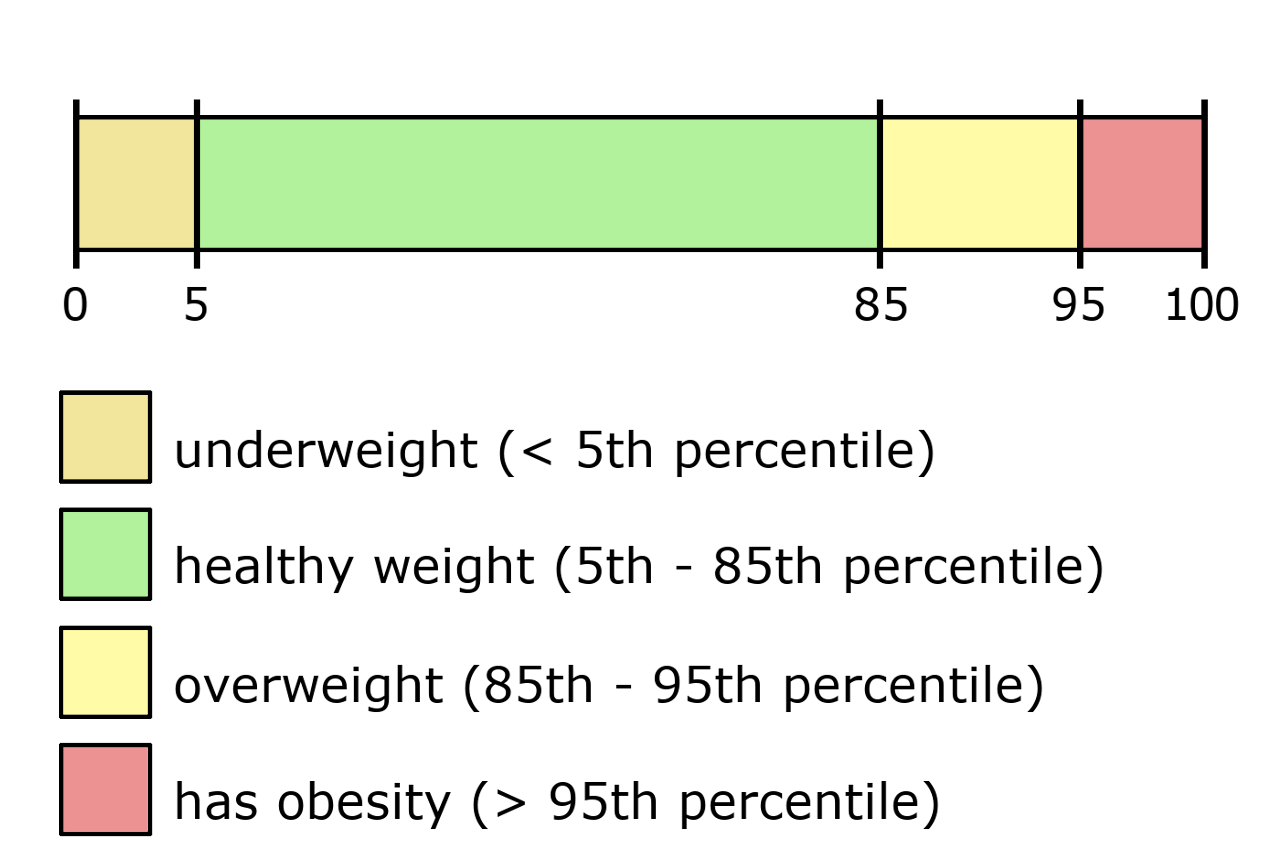
BMI Categories for Children Ages 2-19
| Weight Category | Charting Percentile |
|---|---|
| Underweight | <5th percentile |
| Healthy Weight | 5th to <85th percentile |
| Overweight | 85th to <95th percentile |
| Obese | >95th percentile |
Healthy BMI for Children
A study from JAMA pediatrics found that from 2011 to 2012, 17.3% of children in the United States aged 2 to 19 years were obese. Additionally, 5.9% of children met criteria for class 2 obesity, and 2.1% met criteria for class 3 obesity. In addition, all categories of obesity in children showed an increase over the previous 14 years.[6]
Similar to adults, severe obesity in children is associated with an increased prevalence of heart disease and metabolic risk factors.[7]
In addition, a study from the New England Journal of Medicine also found that children with obesity and its related health issues had higher rates of premature death.[8]
Calculating and tracking BMI in children can be a useful way to diagnose health issues early on to minimize these risks.
A study from the Journal of Pediatrics found that pediatricians that followed children with BMI charting recognized weight issues at a higher rate compared to only utilizing height and weight charting alone.[9]
The nice thing about the BMI formula is that it is quick and easy to calculate. However, since it only uses these metrics, it also has drawbacks.
For example, it does not take lean body mass, physical activity, genetics, or other health conditions into consideration. In older kids and adolescents this may have a bigger influence on weight and body fat and should be taken into account.
By using BMI charts in children and monitoring weight as children age, you can promptly identify disruptions in growth which can help avoid chronic health issues associated with obesity.
Limitations of Body Mass Index
Similarly as with adults, using BMI as a marker for health has limitations.
When interpreting BMI in children, looking at a child’s growth trend may be more beneficial than simply looking at the percentile range that their BMI falls within.
By traditional interpretations, a child with a BMI at the 95%ile would be considered obese. However, according to Ellyn Satter, if the child has consistently been growing at the 95%ile, this would not indicate an issue that warrants intervention.[10]
Ellyn Satter is a Registered Dietitian and Family Therapist who is considered an expert in child feeding. She notes that BMI calculations don’t show actual body fat percentages. Just like with adults, BMI does not account for genetics, heavy bones, or muscle mass, which are all factors that could cause a child to weigh more but do not reflect fat mass.
While there is usefulness in classifying BMI ranges for children, further interpretation needs to be applied to truly assess a child’s health status.
References
- Centers for Disease Control and Prevention, About Child & Teen BMI, https://www.cdc.gov/healthyweight/assessing/bmi/childrens_bmi/about_childrens_bmi.html
- Centers for Disease Control and Prevention, Data Table of BMI-for-age Charts, https://www.cdc.gov/growthcharts/html_charts/bmiagerev.htm
- Centers for Disease Control and Prevention, 2 to 20 years: Boys Body mass index-for-age percentiles, https://www.cdc.gov/growthcharts/data/set1clinical/cj41l023.pdf
- Centers for Disease Control and Prevention, 2 to 20 years: Girls Body mass index-for-age percentiles, https://www.cdc.gov/growthcharts/data/set1clinical/cj41l024.pdf
- Centers for Disease Control and Prevention, Defining Childhood Weight Status, https://www.cdc.gov/obesity/childhood/defining.html
- Skinner, A. C., & Skelton, J. A., Prevalence and trends in obesity and severe obesity among children in the United States, 1999-2012, JAMA pediatrics, 2014, 168(6), 561-566. https://jamanetwork.com/journals/jamapediatrics/article-abstract/1856480
- Skinner, A. C., Perrin, E. M., Moss, L. A., & Skelton, J. A., Cardiometabolic risks and severity of obesity in children and young adults, New England Journal of Medicine, 2015, 373(14), 1307-1317. https://www.nejm.org/doi/full/10.1056/NEJMoa1502821
- Franks, P. W., Hanson, R. L., Knowler, W. C., Sievers, M. L., Bennett, P. H., & Looker, H. C., Childhood obesity, other cardiovascular risk factors, and premature death, New England Journal of Medicine, 2010, 362(6), 485-493. https://www.nejm.org/doi/full/10.1056/nejmoa0904130
- Perrin, E. M., Flower, K. B., & Ammerman, A. S., Body mass index charts: useful yet underused, The Journal of pediatrics, 2004, 144(4), 455-460. https://www.sciencedirect.com/science/article/abs/pii/S0022347604000927
- Satter, E., Your child’s weight : helping without harming : birth through adolescence, Kelcy Press, 2005,


